Key points
- The 2025 measles outbreak is highly contagious, spreading rapidly in schools, public transportation, and doctors’ offices, making early recognition of symptoms critical.
- Measles symptoms include high fever, cough, runny nose, red watery eyes, white spots inside the cheeks, and a distinctive rash that spreads across the body.
- Protection measures include ensuring everyone is up to date on the MMR vaccine, limiting exposure in high-risk settings, and taking swift action if exposed.
- High-risk groups include infants under 12 months, unvaccinated individuals, pregnant individuals, and people with weakened immune systems; timely medical care is crucial for these groups.

The 2025 measles outbreak is proving to be one of the most significant public health challenges of the decade, with confirmed cases reported in over 30 states in just the first quarter of the year. Measles is exceptionally contagious—up to 90% of people exposed to the virus will get infected if they’re not immune, according to the CDC. They explain that because the virus can linger in the air for up to two hours after an infected person has left a room, it spreads rapidly in schools, public transportation, and even doctors’ offices. That’s why it’s critical to act early: recognizing symptoms, understanding vaccine protection, and knowing when to visit urgent care could make all the difference in keeping your family safe.
What is measles and how does it spread?
Measles is a highly contagious viral infection caused by the measles virus (a paramyxovirus of the genus Morbillivirus). It typically begins with cold-like symptoms — fever, cough, runny nose, and red, watery eyes — followed by a distinctive rash that spreads across the body, according to the CDC. While it may seem like a childhood illness of the past, measles remains a serious public health concern, especially during outbreaks like the one in 2025.
The virus spreads primarily through airborne transmission. When someone with measles coughs, sneezes, or even talks, tiny droplets containing the virus can linger in the air for up to two hours, these droplets can also land on surfaces, where the virus may remain active and contagious. Because of this, it’s possible to become infected simply by entering a room where an infected person has recently been — even if you never come into direct contact with them.
Measles has an exceptionally high transmission rate, with a basic reproduction number (R₀) between 12 and 18. That means one person with measles can infect 12 to 18 others in a fully susceptible population, making it far more contagious than most other viral illnesses, including influenza and COVID-19. This underscores the importance of rapid response, vaccination, and public awareness during an outbreak.
What are the symptoms of measles?
Recognizing the symptoms of measles early can help prevent further spread and allow for timely medical care, especially during a widespread outbreak. Measles symptoms typically appear 7 to 14 days after exposure to the virus, and they tend to follow a predictable pattern, starting with general cold-like signs before progressing into more serious and visible symptoms, according to the CDC.
Here are the key signs and symptoms to watch for:
- High fever — often begins mild but can spike to over 104°F (40°C)
- Cough, runny nose, and red, watery eyes — classic early symptoms that mimic a cold or flu
- Koplik spots — small white spots with bluish centers that appear inside the cheeks and are unique to measles
- Rash — a red, blotchy rash that usually starts on the face at the hairline and then spreads downward to the rest of the body
If you or your child develop these symptoms — especially during an active measles outbreak — it’s important to avoid public places and contact a healthcare provider right away to discuss testing, treatment, and next steps.
How to protect your family during the measles outbreak
Prevention is the most powerful tool we have in slowing the spread of measles, especially during an outbreak as widespread and contagious as the one in 2025. Since measles spreads through the air and remains viable on surfaces, even brief encounters can lead to infection. Fortunately, there are clear steps families can take to stay protected and reduce the risk of transmission.
Here’s how to safeguard your household:
- Make sure everyone is up to date on the MMR vaccine. The measles, mumps, and rubella (MMR) vaccine is about 97% effective after two doses. Children typically get the first dose around 12–15 months and a second at 4–6 years. Adults unsure of their vaccination status should consult their provider — some may need a booster.
- Limit exposure in high-risk settings. Avoid crowded places like airports, malls, and large gatherings when possible, especially with unvaccinated children or immunocompromised family members. Encourage proper hygiene, like frequent handwashing and mask use, if someone in your community is sick.
- Take swift action if you’ve been exposed. If someone in your household has been near a confirmed case, contact your healthcare provider immediately. They may recommend post-exposure prophylaxis or close monitoring for symptoms, depending on vaccination status and health risks.
Staying informed and proactive can go a long way in keeping your family safe during this outbreak.
Who is most at risk during a measles outbreak?
While measles can affect anyone who isn’t fully protected, certain groups face a much higher risk of severe complications, including hospitalization, pneumonia, encephalitis, or even death. Understanding who is most vulnerable during a measles outbreak helps families and communities take extra precautions to protect those who need it most.
The highest-risk groups include:
- Infants under 12 months – Babies are too young to receive their first dose of the MMR vaccine and rely on herd immunity for protection.
- Unvaccinated children and adults – Whether due to medical, personal, or access-related reasons, those who haven’t received the full MMR series are significantly more likely to get infected and spread the virus.
- Pregnant individuals – Measles during pregnancy can lead to complications such as miscarriage, premature birth, or low birth weight.
- People with weakened immune systems – This includes individuals undergoing chemotherapy, taking immunosuppressive medications, or living with conditions like HIV/AIDS. They may not be able to receive the vaccine and are more prone to life-threatening complications.
For these groups, community-wide vaccination and rapid response to potential exposure are especially critical.
When should you seek medical care for measles symptoms?
Timely medical care can make a critical difference when it comes to measles, especially for children and other vulnerable individuals. While many cases resolve on their own with rest and fluids, some symptoms signal more serious complications that require urgent attention, according to the CDC. If you or a loved one shows any of the following warning signs, don’t wait — reach out to a healthcare provider or visit an urgent care center promptly.
Watch for these red flags, listed by the CDC:
- Persistent high fever — especially if it lasts more than a few days or exceeds 104°F (40°C)
- Difficulty breathing — including rapid breathing, wheezing, or shortness of breath
- Signs of dehydration — such as dry mouth, reduced urination, dizziness, or extreme thirst
- Seizures or extreme lethargy — any loss of consciousness, unresponsiveness, or unusual confusion
Seeking care early improves outcomes and helps reduce the spread to others, especially in clinics equipped to safely isolate contagious patients. For most measles symptoms — like mild fever, rash, or discomfort — urgent care is a convenient and effective option for evaluation and treatment. However, if symptoms are severe, such as trouble breathing, seizures, or signs of severe dehydration, head straight to the emergency room. When in doubt, call ahead or use a telehealth visit to determine the safest next step for your situation.
How is measles diagnosed and treated?
Measles is usually diagnosed through a combination of physical symptoms, like the characteristic rash and Koplik spots, and confirmation with a lab test, such as a blood sample or throat swab. Healthcare providers may also ask about recent travel, vaccination status, or known exposure to someone with measles. While there’s no specific antiviral “cure” for measles, treatment focuses on relieving symptoms and preventing complications, according to the CDC.
Supportive care may include:
- Hydration to prevent or treat dehydration caused by fever and poor appetite
- Fever reducers like acetaminophen (Tylenol) or ibuprofen to ease discomfort (never give aspirin to children with viral illnesses)
- Vitamin A supplements, especially in children, which have been shown to reduce the severity of measles-related complications. Vitamin A is a fat soluble vitamin and excess doses stay in the body and can harm it. Appropriate dosing is crucial to avoid toxicity.
With close monitoring and early care, most people recover fully, but high-risk individuals may need hospitalization for further support, according to the CDC.
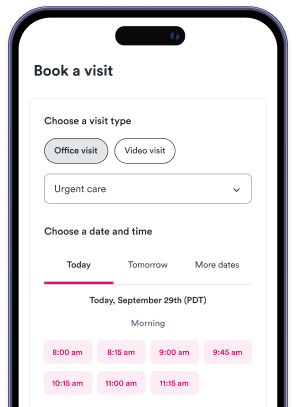
Find urgent care near you if you suspect measles symptoms
If you or your child are showing signs of measles, like a persistent fever, rash, or cough, it’s important to get medical guidance as soon as possible. Visiting an urgent care clinic can help you confirm a diagnosis, manage symptoms, and prevent further spread. Don’t wait and wonder — use Solv to find an urgent care near you and book a same-day appointment in your area. It's fast, convenient, and designed with your family's health in mind.
FAQs
What is measles and how does it spread?
Measles is a highly contagious viral infection caused by the measles virus. It begins with cold-like symptoms such as fever, cough, runny nose, and red, watery eyes, followed by a distinctive rash that spreads across the body. The virus spreads primarily through airborne transmission. When someone with measles coughs, sneezes, or talks, tiny droplets containing the virus can linger in the air for up to two hours, and can also land on surfaces where the virus remains active and contagious.
What are the symptoms of measles?
Measles symptoms typically appear 7 to 14 days after exposure to the virus. They start with general cold-like signs before progressing into more serious and visible symptoms. These include high fever, cough, runny nose, red, watery eyes, Koplik spots (small white spots with bluish centers that appear inside the cheeks), and a red, blotchy rash that usually starts on the face at the hairline and then spreads downward to the rest of the body.
How can I protect my family during a measles outbreak?
To protect your family during a measles outbreak, make sure everyone is up to date on the MMR (measles, mumps, and rubella) vaccine, limit exposure in high-risk settings, and take swift action if you've been exposed. If someone in your household has been near a confirmed case, contact your healthcare provider immediately. They may recommend post-exposure prophylaxis or close monitoring for symptoms, depending on vaccination status and health risks.
Who is most at risk during a measles outbreak?
Certain groups face a much higher risk of severe complications from measles, including hospitalization, pneumonia, encephalitis, or even death. These high-risk groups include infants under 12 months, unvaccinated children and adults, pregnant individuals, and people with weakened immune systems.
When should I seek medical care for measles symptoms?
Timely medical care can make a critical difference when it comes to measles. If you or a loved one shows any of the following warning signs, reach out to a healthcare provider or visit an urgent care center promptly: persistent high fever, difficulty breathing, signs of dehydration, seizures or extreme lethargy. If symptoms are severe, such as trouble breathing, seizures, or signs of severe dehydration, head straight to the emergency room.